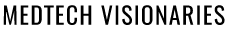
For severe heart failure patients, an LVAD, or left ventricular-assist device, helps the heart pump blood. 7asmin via Wikimedia Commons
For those suffering from Dead Heart Muscle, heart transplants soon be a thing of the past –
a Closer look at LVADs
by Lisa O’Keefe
If you suffer from heart muscle death you are also most likely dealing with a level of anxiety over your condition. The first question you might wonder is “what percentage of my heart is affected”. To answer that question your doctor would need a Cardiac MRI or PET so your doctor can estimate what percent of the heart muscle has been replaced by a scar.
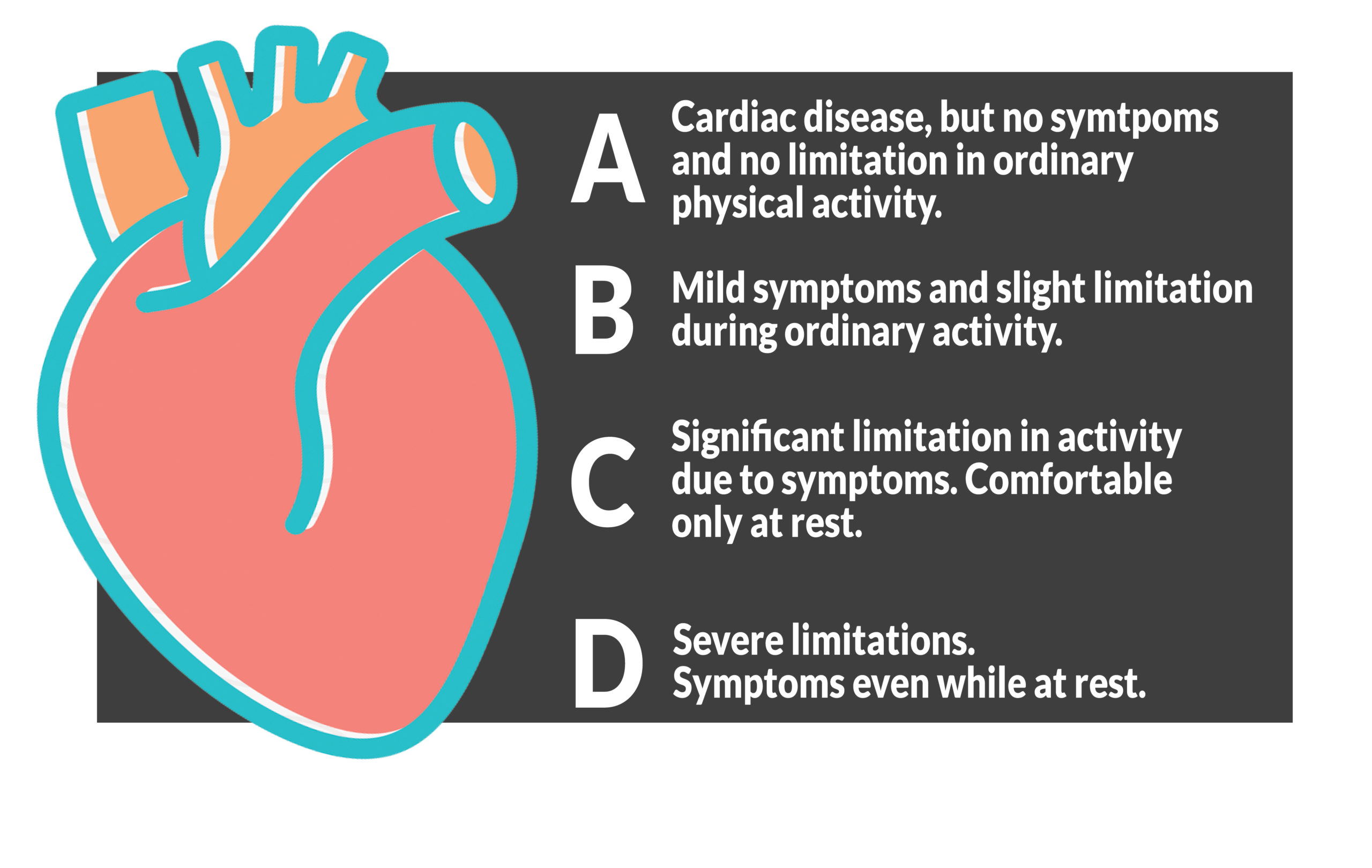
The 4 stages of heart failure
 The second question you might have is “what is out now in the MedTech field that can help me live a longer, healthier life”. And the fast answer is that there are a number of conventional and emerging technologies that are addressing that concern including stem cell, patches, PRP injections and VADs for biventricular dysfunction – all of which will be addressed in future articles. But in this article, I want to focus on two of the more established technologies – heart transplants and LVADs. And to get a better understanding of these technologies I virtually interviewed one of the leading experts in this field Dr. Larry Allen. Globally respected for his work with Advanced Heart Failure and Transplant. Dr. Allen is a Professor of Medicine-Cardiology at the Colorado University School of Medicine and Associate Head, Clinical Affairs, Cardiology Director at the Advance Heart Failure at the UCHealth Heart Failure Program – Anschutz and Heart & Vascular Center – Anschutz.
The second question you might have is “what is out now in the MedTech field that can help me live a longer, healthier life”. And the fast answer is that there are a number of conventional and emerging technologies that are addressing that concern including stem cell, patches, PRP injections and VADs for biventricular dysfunction – all of which will be addressed in future articles. But in this article, I want to focus on two of the more established technologies – heart transplants and LVADs. And to get a better understanding of these technologies I virtually interviewed one of the leading experts in this field Dr. Larry Allen. Globally respected for his work with Advanced Heart Failure and Transplant. Dr. Allen is a Professor of Medicine-Cardiology at the Colorado University School of Medicine and Associate Head, Clinical Affairs, Cardiology Director at the Advance Heart Failure at the UCHealth Heart Failure Program – Anschutz and Heart & Vascular Center – Anschutz.
And now that you know a bit more about Dr. Allen let’s look at what he had to say and the resources he wants to share with you so you can better understand some of the options you can discuss with your doctor regarding dead heart muscle. One option is a heart transplant. “Heart transplants have been the go-to for a number of years and has significant data regarding the results to back its progress,” said Dr. Allen. “If you would like to see the data please go to https://www.srtr.org/transplant-centers/?organ=heart&recipientType=adult&query= This website will show transplant results by state, or nation, depending on the filters you add”. It also documents the continual increased survival rates for those with a heart transplant.
But heart transplants are not the only option and according to Dr. Allen LVADs may be the new future. LVAD stands for Left Ventricular Assist Device. This device is for those with advanced heart failure (Class C or D) who meet certain criteria. One of the success stories with LVAD can be found here https://www.9news.com/article/news/health/i-figured-i-was-dying-innovative-heart-pump-gives-colorado-man-new-life/73-5c149137-f4fa-4a82-8c91-8d8be178964e In that article, the patient, Mr. Phillips, was dying of heart failure. Fortunately, he was lucky enough to be in the hands of Dr. Allen and UCHealth, which at the time was the only hospital in Colorado, New Mexico, and Wyoming providing heart transplantation and artificial heart devices. (New Mexico Heart Institute has since opened an LVAD program last year.) Phillips received his LVAD on July 11, 2011 and in 2019 underwent a transplant.
Now before I go further, I want to stress that LVADs are for the left ventricle and not for when someone needs a VAD for biventricular dysfunction. Biventricular dysfunction will be covered at a later date. This device, the LVAD device, acts as a suspended pump next to the heart. It is inserted into the chest and then the driveline cord connects the pump to the outside. A computer controller operates the pump and displays messages and sounds alarms about the device. The pump motor is placed inside the chest and allows the blood to flow into the left ventricle of the heart then into the inflow cannula and then into the pump in a continuous and seamlessly undetectable movement. This pump not only improves and regulates blood flow but also improves the quality of life. And according to Dr. Allen, these heart devices are now almost as good as a transplant in terms of survival rate and virtually eliminates clot formation and significantly reduced strokes.
So what are the concerns?
According to Dr. Allen “Heart replacement therapies (LVAD, transplant) work best when the heart is the only problem. Everything else is/can be a distraction, impede care, and limit response to treatment.” As for side effects, it depends “on the therapy. There is always a risk with any surgery and there is the immunosuppression factor and possible bleeding, clotting, and infection for LVAD.” The recovery can be long and hard with most patients staying in the hospital for a couple of weeks or longer. Some people may need to be readmitted. A low percentage of people may have serious bleeding or have a stroke.
When discussing success rate Dr. Allen says “we have developed some materials that describe outcomes for LVAD to help patients decide if this is something they would want to pursue: https://patientdecisionaid.org/lvad/” I totally love this website. It is designed for people like you and me who do not have any medical background. Everything is laid out in pictures, videos, bullet points, and booklets. The website gives you treatment options to think about and discuss with your health care provider regarding the risks and benefits of “available treatments and to empower patients to become more involved in the decision-making process.” In this website, it mentions that LVADs are used for two basic reasons – either to treat people until they can secure a heart transplant (called BTT or bridge to transplant) or it is used to treat people, over their lifetime, who have severe heart failure and cannot get a transplant (called destination therapy or DT). For both BTT and DT the surgery, types of device, and recovery are the same. The website explains the process for getting an LVAD, what complication might occur, how you will feel, and the possible survival rate from an LVAD process (as a hint 9 out of 10 patients who got an LVAD are still alive after 1 year and some with LVADs have lived 13 years.) And it even lets you know more about the cost, which depending on your insurance coverage, may have extra costs with your device. Many patients have to pay for the driveline bandages. You may also have co-payments for your medical care.
I do hope this information has helped. I want to thank Dr. Allen and UCHealth for providing this information to better help you understand the advances in the MedTech field with dead heart muscles. Please always remember to educate yourself on all options available so you can discuss with, and seek the advice of, your own doctor who best understands your own personal medical needs.